Those of us who have been very cautious throughout the pandemic are seeming to catch the more recent variants of the SARS-COV-2 virus, also known as COVID, myself included. I knew it was only a matter of time, and the timing for me was a big bummer because it came right before Friends for Life Orlando. So, for the first time since FFL Orlando 2000, the very first Friends for Life, I did not attend the conference.
I hope that sharing my COVID experience, as well as my experience with the medication, Paxlovid, as a person living with type 1 diabetes, will help others navigate their experiences. This current variant seems to be spreading quickly and even among people who are fully vaccinated, so I also recommend keeping an eye on your symptoms and getting tested if you experience any. Luckily for me, my symptoms were mild, I caught it early, and got a prescription for Paxlovid right away.
What is Paxlovid?
Paxlovid is an oral treatment, meaning a pill you can take, for COVID-19. It’s not recommended or even available for everyone, but you can ask your doctor about getting a prescription, if you weigh at least 88 pounds (40 kg).1 The guidelines are that you need to start it within five days of testing positive for COVID, and most people will only recommend taking it if you are at high risk for poor outcomes with COVID.1 This means if you have diabetes, you may qualify.
Paxlovid is a combination anti-viral medication with one part that stops the virus from being able to make parts that it needs to survive and another part that helps keep the anti-viral medicine in the body longer, allowing it to work fully. After the virus is stopped from making parts it needs to survive, the virus that’s left in the body cannot enter new cells, which stops the infection of the virus.1 This can mean that Paxlovid may shorten your infectious time and it helps keep symptoms more mild.
What are the Possible Benefits of Paxlovid?
The studies that allowed Paxlovid to get approved by the FDA showed that it reduced the risk of hospitalization and death by 89%.1-2 The study looked at 2,200 people who were unvaccinated and experiencing symptoms of COVID. It can also keep symptoms in the more mild stages when taken at the start of the viral course, and shorten the time frame of infection.
What are the Possible Side Effects of Paxlovid?
Most of the side effects that people experience are mild and are:1-2
- Altered sense of taste
- Diarrhea or nausea
- Muscle aches
- Increased blood pressure
There have also been some reports of people who get a “rebound” after taking Paxlovid, when symptoms and positive results resume a short time after completing the drug. It does not happen for everyone, but it is something to be aware of – especially if you are considering attending a large in-person event, I don’t know, maybe something like Friends for Life…Which is another reason I chose to stay home, because I did not want to expose 1,800 people with diabetes to COVID. (Insert crying face)
Paxlovid and Diabetes:
There is not a whole lot of information about Paxlovid for people with diabetes, and studies are still ongoing to see how Paxlovid works for people with diabetes. There are a number of medications that interact with the anti-viral medicine such as statins, which are very commonly used for high cholesterol.1 It is also not recommended for people with moderate to severe kidney disease, which is more common for people with diabetes.
I’m hoping that sharing my personal experience will help you if you experience COVID with diabetes, and help you decide whether or not to ask your healthcare team about trying Paxlovid. This is just my personal experience, and in the interest of giving you the full picture, I am fully vaccinated with two boosters, I have no other underlying chronic conditions, my kidneys are healthy, I am not pregnant or breastfeeding, and I do not take a statin.
Here’s my timeline of COVID:
Sunday 6/25
Husband finds out family has positive cases that he saw Friday 6/23
Does home antigen test: very faint positive
Symptoms: none aside from fatigue
Instantly puts on mask and I look for hotels to avoid the rest of us getting COVID
Within two hours he is out of the house and I am disinfecting all of the surfaces of the house
Monday 6/26
Husband had chills overnight, body aches, no appetite (his loss of appetite is honestly still happening as I write this article a couple weeks later)
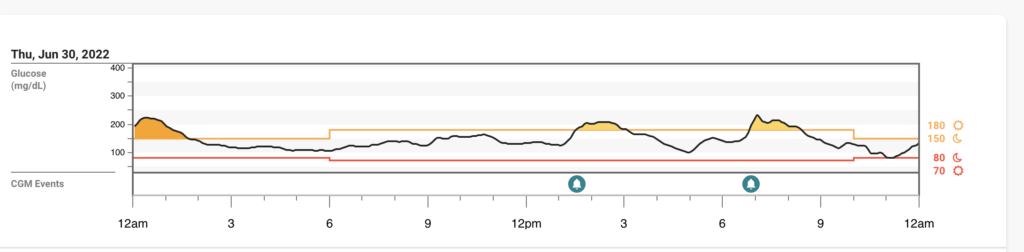
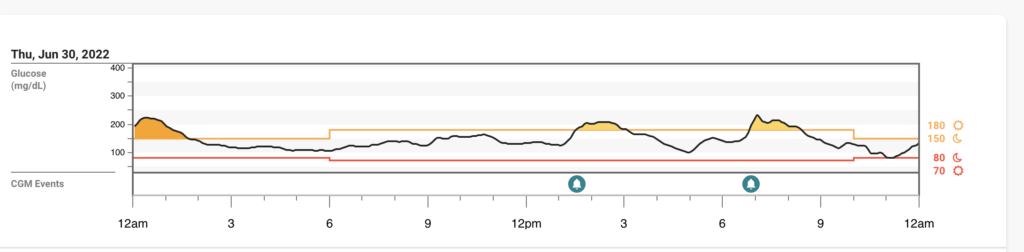
Thursday 6/30
Home COVID test for me: again very faint positive
Symptoms: slight runny nose and anxiety that I won’t be able to attend FFL
Reached out to my friends with diabetes who have taken Paxlovid to see if I should ask for RX
Sent MyChart message to my doc asking for Paxlovid prescription (RX) if my PCR is positive
CVS drive through Antigen: negative
PCR: also negative
Blood Glucose Levels (BG’s): Looking pretty darn good if I do say so myself
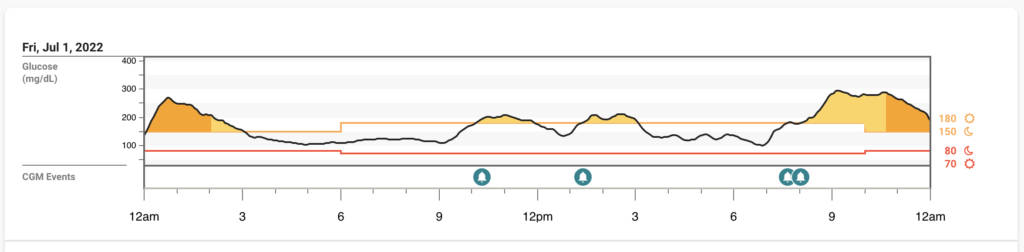
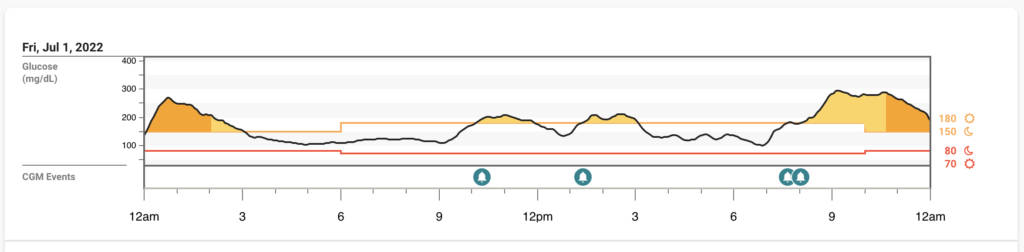
Friday 7/1
Symptoms: Woke up with a sore throat and a cough, realize I’m not going to make it to FFL
Home COVID test: Instantly positive
MyChart message to doc: Sends RX to pharmacy within 10 minutes
Husband OK’d to return home, his symptoms have mostly resolved
We kept masks on inside while around the kids and ate outside or in different rooms
Started Paxlovid after dinner Friday evening: Instant side effect of metallic taste in mouth
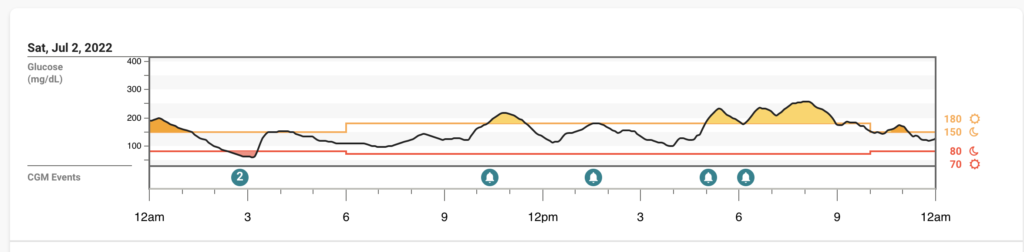
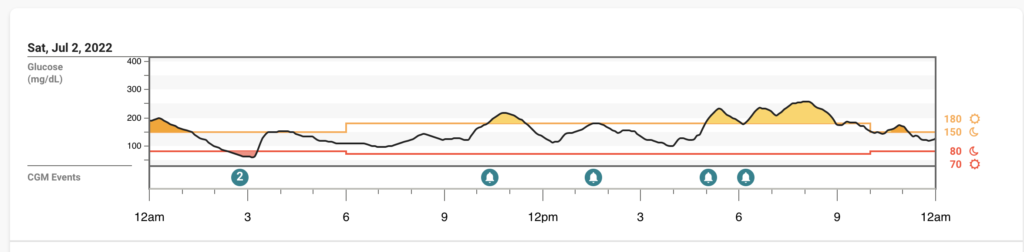
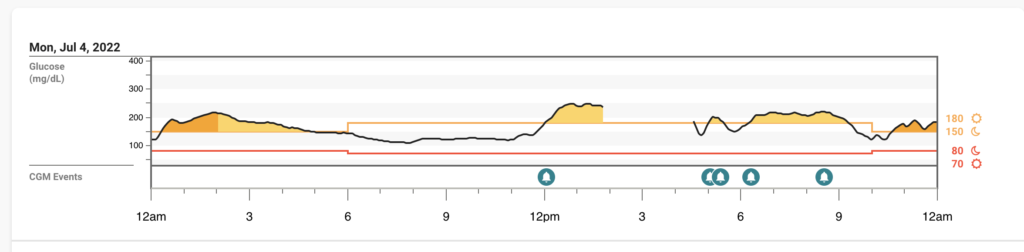
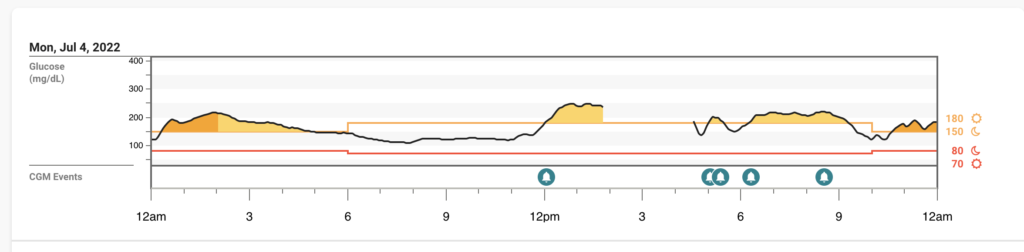
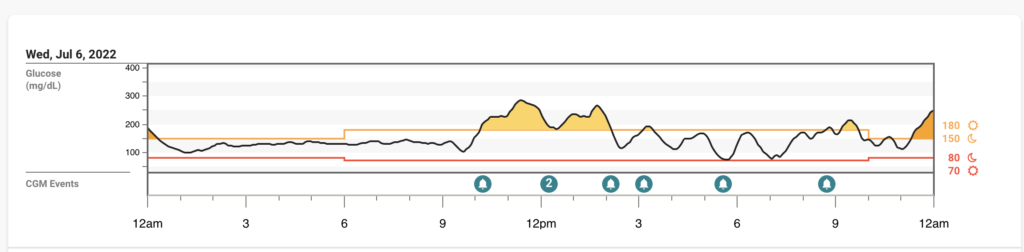
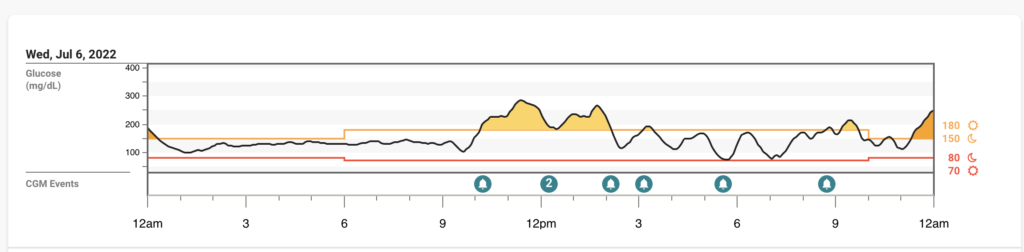
BG’s: I had some highs overnight, and then again when I started Paxlovid (see CGM Tracing)
Saturday 7/2
Symptoms: Runny nose, sore throat, less of a cough, no fever or chills, just tired and my body ached all over
Slept as much as I could, blood sugars were honestly less crazy than I expected
Taking Paxlovid, still experiencing the metallic taste, but not that bothered by it, still maintaining a normal appetite, and drinking lots of Gatorade and water.
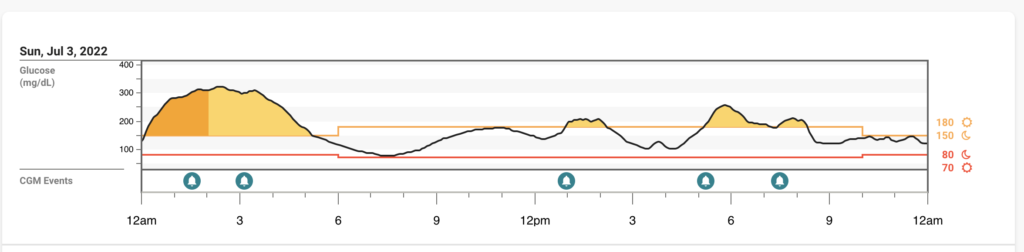
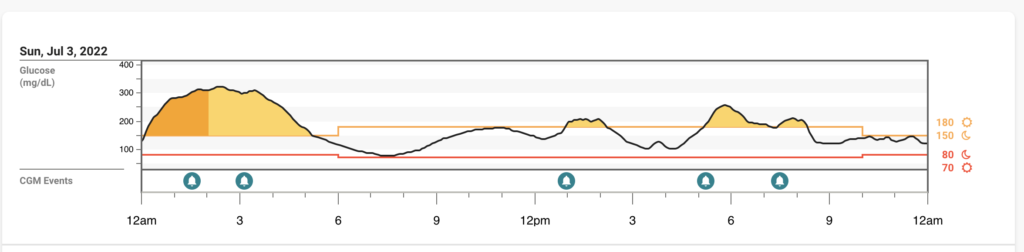
Sunday 7/3
Symptoms: EXHAUSTION – slept for 12 hours this night! I was also told by a friend that the long-COVID symptoms were associated with sleep disturbances or sleep loss during COVID so I decided to SLEEP! And luckily by then my husband was feeling well enough to care for the kids.
Monday 7/4
Symptoms: At this point, I felt honestly pretty normal. I even felt well enough to do some cleaning, which was surprising, but I was happy to have some energy back.
BG’s: Not much to complain about overall, especially after how high I was the night before I was happy to be more in range.
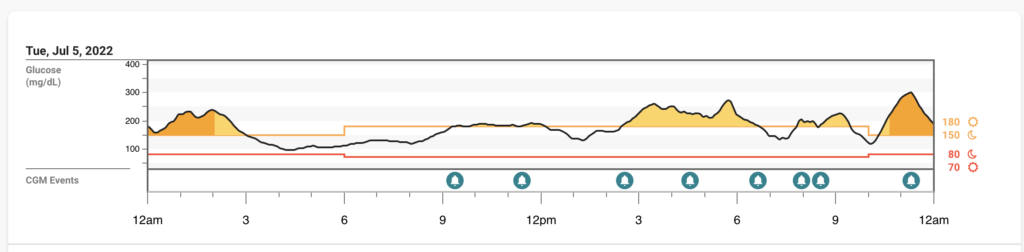
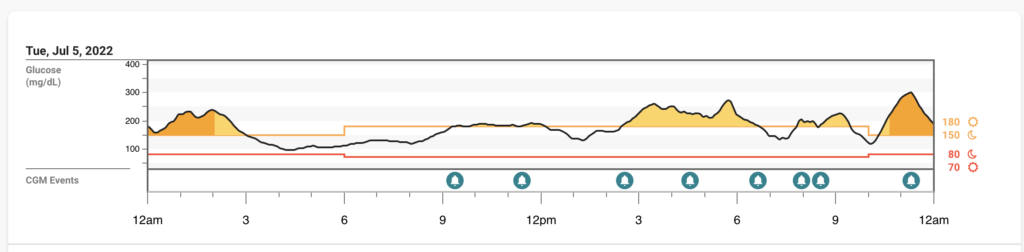
Tuesday 7/5
Symptoms: Back to baseline at this point
BG’s: Interestingly high a lot of today, but I’m wondering if it was added stress of not being at FFL and trying to help from afar…also last dose of Paxlovid was this evening
Wednesday 7/6
This is really intriguing to me – BG’s were pretty decent today, no symptoms, and I’m assuming Paxlovid still a bit in my system but the two days that follow are much more volatile BG wise.
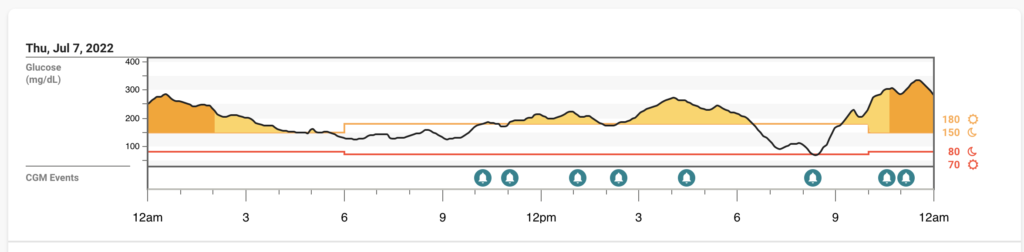
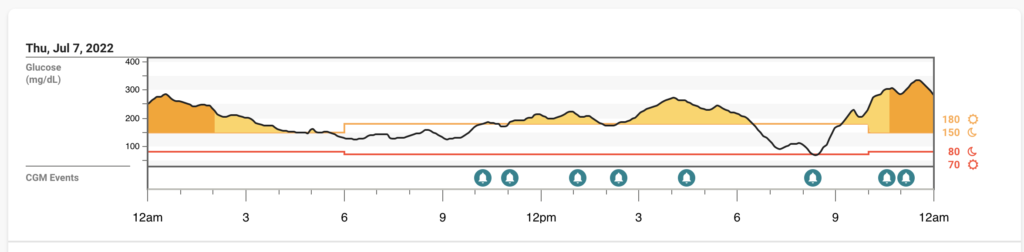
Thursday 7/7
Friday 7/8
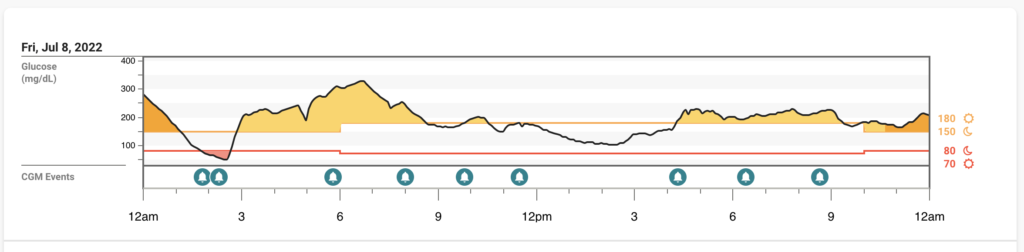
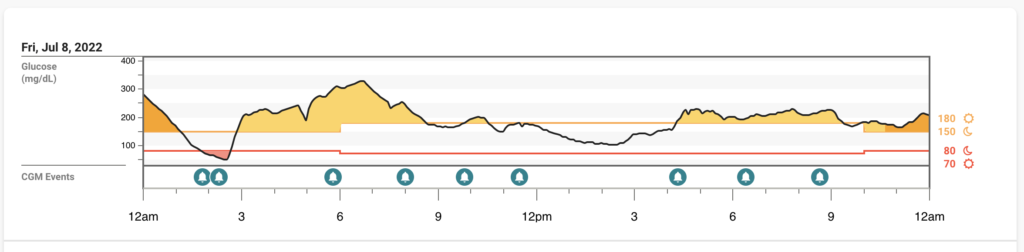
Overall, I was very happy with my experience with Paxlovid and felt very lucky that my doc prescribed it so quickly for me. It’s hard to tell what the higher percent time high was caused by on these days – it could have been a slight rebound from the Paxlovid, it could have been the stress of helping trouble shoot FFL issues from afar, and I’ll never really know. I have also heard from others who have T1D and gotten COVID that their blood sugars were elevated much more than I seemed to experience, and they used temporary targets or increased temporary basal rates to help.
Paxlovid Rebound?
I did experience a sore throat Sunday 7/10, and I just had tea with honey and took some ibuprofen. Then, the next couple of days after that I felt that I was experiencing what I will call “brain fog” where it felt like my brain just wasn’t working like it normally does. I also had a night where I woke up from 11:45 PM – 3:45 AM which is very abnormal for me, usually I can fall right back asleep.
Do I know if any of these are related to my COVID experience, to Paxlovid, or just happen to be around the same time? No idea, honestly. But this was my experience and I hope it helps someone else navigate theirs.
Written and clinically reviewed by Marissa Town, RN, BSN, CDCES



