People with diabetes are often turning to continuous glucose monitoring (CGM) to help improve their diabetes management. The technology has improved dramatically since the first CGM was on the market in the early 2000’s and has been proven in studies repeatedly to help improve glycemic control for people with diabetes.1,2
When the first commonly used CGMs were available to patients in the U.S., each company had their own proprietary software that would allow people with diabetes and their health care teams to review their CGM Data. This became a barrier in a couple of major ways.
First, if you wore a CGM, you would have to download the proprietary software and use a proprietary plug to be able to upload your data at home, and this is also assuming you have a working computer. Second, for the healthcare teams, the providers would have to learn how to interpret the various upload reports and the clinic staff would have to have the ability to upload to the various software on the clinic computers with the correct cords. Or you could paper log like it was 1989…
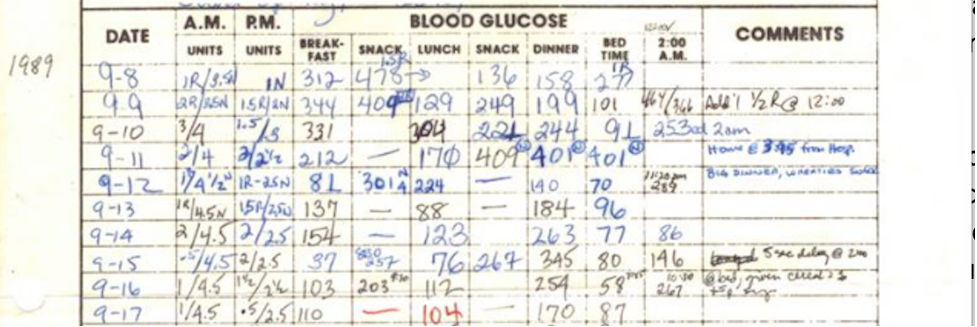
Diabetes Mine published an article on Healthline in July 2019 about reviewing data with your healthcare team, which further emphasizes the need for a better way to get data from our diabetes technology devices. Their article suggests printing out reports of your diabetes data to bring to your doctor’s office, something with which I am familiar.
With my personal endocrinologists, they always loved having my print outs when they didn’t have the latest software for my devices. But, printing required extra work on my part. And when I took it to my high-risk OB/Gyn when I was pregnant, the doctor had no idea what to even do with the data. He had never seen a Dexcom on a patient, much less a printout with all of the data points.
What is interesting to me, as a nurse, is that there are no other medical devices that I am aware of that have their own proprietary data reporting. For example, if you go to the hospital with chest pain, you will get an EKG (electrocardiogram). The EKG machine will then print out a standardized report so that the health care team can easily interpret the data and make treatment decisions.
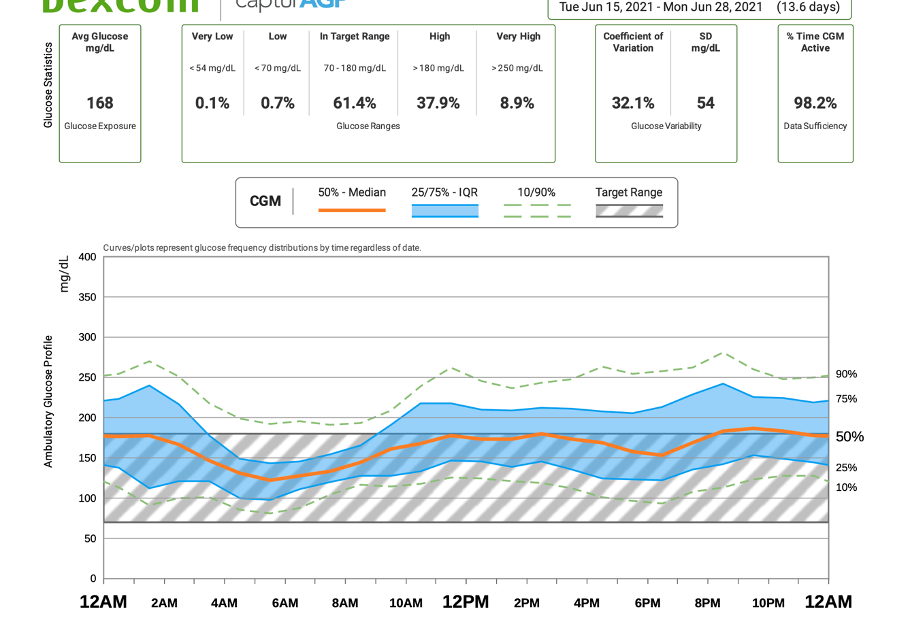
After 23 years of having CGMs, we have arrived at a standardized report called the Ambulatory Glucose Profile (AGP).3 What helped the AGP come to fruition was work by many healthcare providers, diabetes organizations, and industry partners coming together to decide what they felt would be the best reporting method, presenting it to the FDA, and the FDA, in turn, presenting this to all of the CGM manufacturers to incorporate in their software.3
Another piece of the puzzle was healthcare professionals across the world coming together for a consensus statement on CGM use.4 Out of this consensus statement came targets for CGM metrics, which had not been previously established by any diabetes organization.4 The AGP shows these metrics at the top of the report.3
Additional features of the AGP are:
- Target glucose ranges
- Target for percent time in range, time above target, and time below target
- Average glucose and estimated HbA1C
- A graph with the median 50% of blood glucose range, highlighted with the target range outlined
- Daily glucose profiles in snapshots below the larger graph
Here are two examples of what you can find in an AGP from the Dexcom Clarity software below.
Hopefully the AGP being in all software systems for all diabetes technologies will decrease barriers for healthcare providers prescribing or offering devices to their patients. It may also help both people with diabetes and HCPs make meaningful changes based on the data. The next recommendation by the authors of the Standardized Reporting article is to streamline integration into electronic medical records.3
One day, we will look back at this and think of how much better we have it, but until then, this is the best we’ve got. And I, for one, am grateful for my diabetes technology!
- Effect of Continuous Glucose Monitoring on Glycemic Control in Adolescents and Young Adults with Type 1 Diabetes: A Randomized Clinical Trial, June 2017, Diabetes Technologies & Therapeutics
- Effects of Continuous Glucose Monitoring on Metrics of Glycemic Control in Diabetes: A Systematic Review with Meta-Analysis of Randomized Controlled Trials, May 2020, Diabetes Care
- Beyond A1C – Standardization of Continuous Glucose Monitoring Reporting: Why it is needed and how it continues to evolve, May 2021, Diabetes Care
- International Consensus on Use of Continuous Glucose Monitoring, December 2017, Diabetes Care
Written and clinically reviewed by Marissa Town, RN, BSN, CDCES


