Julie Rubis
The following is a post I made to celebrate National Diabetes month as an education piece for friends and family.
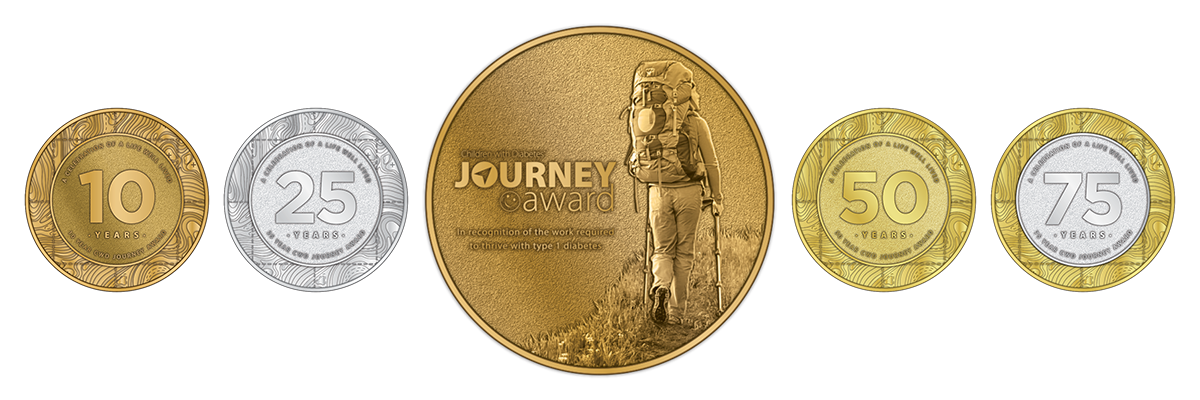
July 2025 will mark my 53rd year of being a Type 1 Diabetic. My journey of 50+ years is a lot to cover, but my hope is you’ll get a glimpse into the life of a diabetic and hopefully learn something along the way.
I was 7 years old when Dr. Richard Bickham shared the news with me and my parents in his office in Allen Medical Building in Bay City, MI. I can still picture his big leather office chair and my mom, dad and I being told that I needed to go to the hospital immediately because I had “sugar diabetes”. I remember my mom crying and my dad looking perplexed. None of us knew what my new reality would be and this diagnosis happened just three years after my brother had passed away. As a parent, I cannot fathom the stress my poor parents had at that moment and the amount of worrisome years to follow.
It hasn’t been an easy road, but it could have been so much worse. I’d like to tell you every day got a bit better. But merely, some days are better than others. Some days I can do no wrong and my sugar levels remain steady. On other days, I think I am doing everything right, but my glucometer’s high sugar level readings display otherwise.
There are more variables than I can count that affect sugar levels; such as the type of food you eat (not just foods with or without sugar), the time of day, your activity, stress levels, a cough, the flu, and a million little things. For example: The Dawn-Phenomenon is a rise in blood sugar levels that occurs in the morning, usually between 2–8 AM. During this phase, your sugar level goes up without much explanation, but you must account for it. There is a similar phenomenon called, Foot to Floor phenomenon where your sugar level goes up once your feet hit the floor in the morning. These don’t consistently occur every morning, either. There are also so many fluctuations and you just don’t know why.
I originally started out injecting insulin and peeing in a cup to test my sugar levels. My first independent injection was given to me at Mercy Hospital, it was just two units of this stuff called insulin. I practiced giving shots to an orange. The skin of an orange peel had a similar texture to that of a person’s skin. I was a 7 year old who left the hospital knowing how to do injections because I wanted to avoid having to ever go back there. After years of injections my schedule changed to 2 injections daily, then 4 and then 6 a day. I was literally a pin cushion up until my late teens when I started using an insulin pen.
These “pens” were pre-filled with fast-acting insulin that I’d take with meals and snacks or to make adjustments if my sugar level was high. I took another type of insulin before bed that was long-acting. Together, both became the treatment, or therapy as it is called, to help me manage my sugar levels from consistently being too high. I used to say I was “shooting up” which was not a good thing to say when you’re a teenager. It was “I’m high so I need to shoot up” 🤣.
In the late 1990’s I took a chance and started on insulin pump therapy. It was like winning the lotto, one poke every three days – a small cannula remained in my body. The freedom of the pump allowed me to have an amazing corporate job, travel the world alone and basically be “normal”… without having to eat on schedule.
I have been blessed by avoiding spending time in a hospital (for diabetes). With the exception of when my dad passed away and I started beating up my mom unknowingly because my glucose level (blood sugar) was so low due to stress. It happened again the night of my 25th class reunion when I was on the planning committee and had a little too much, danced all night and didn’t eat. When later at home that night my glucose level went down to 10 and I was non responsive and was revived by a volunteer fireman (my neighbor who was a mortician). The first thing I asked him was “did I die”. Kinda funny now…
Luckily, I haven’t had to experience that again. I don’t ever want to.
An insulin pump acts more like a person’s pancreas. Essentially, a pump continues to add insulin to your body every few minutes, which is easier on your body than the infrequent ‘bursts’ of insulin from an injection. It can help you (better) maintain consistent sugar levels, in addition to dosing for meals and snacks.
I also have a continuous glucose monitor (CGM) which measures my sugar levels in (almost) real-time and displays them to me on my phone so I can make adjustments as needed versus waiting to prick my finger and then adjust. So if I’m ever with you and am looking at my phone I’m most likely tending to my diabetes… but okay sometimes I may not be 🤣.
A CGM helps a diabetic get a better picture of how their overall glucose levels are. For an average of 90 days there is a test called an A1C. A non-diabetic’s A1C is between 4 and 5.6. Over the years, my A1C has ranged much higher but I am really close to being at 6.9 for the first time in my life. This is a personal win for me and continues to go lower which is one of the better results a diabetic can get. I can still get better, but I could still do a lot worse than I have in the past.
When my sugar level is low (when a blood-glucose level is less than 70 mg/dL) – it is no fun, you feel like you are living in slow motion, you get confused, you shake, and your body craves sugar like a deprived 5-year-old let loose in a candy store. It’s hard to adequately describe what a low actually feels like because the feeling ranges. Sometimes when you are low, you can consume an all-you-can-eat-sugar buffet in 15 minutes before you’ve become an overachiever and then your glucose level goes too high. But in that moment, anything is better than feeling low. Anything.
My go-to low treatment is glucose tablets, Skittles or chocolate milk. Even after 50+ years and what seems like hundreds of times facing this unnatural feeling, I still consume too much sugar and then I’m too high. The roller-coaster of high to low to high totally wears me out.
My CGM will alert my pump to alert me that I’m trending low, but sometimes I can also feel a low approaching so I can begin treating sooner..
Some Type 1 diabetics have dogs trained to sense when they are high and low. Not that she is a trained dog, but I truly feel Lola “knows” when my sugars are off. She often comes to sit by me and looks at me for a while as I eat my glucose tablets… but she could be just asking for a treat too.
Sometimes the insulin pump acts like it works, but while changing out the tubing and inserting a new needle, the needle can get bent or something else can go wrong. It doesn’t tell you because it doesn’t know, so then my glucose level is higher than I should be. That’s the worst. You know you are doing everything right, but your levels aren’t coming down despite giving yourself enough insulin to overdose. It is frustrating.
Being diabetic you need to know math… and I’m not good at math 🤣 but every ounce of food you consume needs to be calculated for. The beauty of a pump, once your initial settings are set you simply have to enter the number of carbs you are eating and it will calculate the dose for you. A good sugar level range for me is 80-150. But, unfortunately, the pump doesn’t always get it right.
Insulin on board. Even though the insulin is, “fast-acting” it still takes a few hours to get through your system.
High sugar levels, on the other hand, make you feel generally sick and nauseous, headache, crabby/mean and exhausted. It sometimes leaves a weird taste in your mouth, as if extra sugar is spreading anywhere it can go since you have too much in your system and not enough insulin to, “eat it up.” I haven’t been experiencing too many “highs” lately, but they do happen from time to time despite my (best) efforts to keep them in check.
Constantly high sugar levels and high A1Cs are where diabetic complications arise. As for me, I have been very blessed with minimal complications of having this autoimmune disease for so long. Some stomach issues and just within the past couple years with retinopathy in my eyes. Thank the Lord my eyes are currently in great control thanks to some amazing medical advancements. I’m currently fighting my insurance to continue to cover these injections that cost $10k+ a shot!
I truly believe my positive attitude and believing that nothing can stop me has helped me in my diabetes “journey”.
There is always talk of a cure, pancreas transplants, capping the price of insulin, and even using stem cells to reboot the pancreas. While I hope there will be major medical advancements in the next few years, if not a cure, I’m thankful for the technology currently available, which allows me to use a combination of the insulin pump and CGM to sustain me. This technology allows me to live pretty close to normal life. And for a few hours a day, I can forget I have diabetes, or as the late actor Wilford Brimley pronounced it, “diabeetus.”
I will conclude with a current platform from a Diabetes pump supplier…
Think of Type 1 this way. Living with diabetes is a constant balancing act. It’s like doing everything in your daily life while keeping a balloon in the air.
For those of you who have read this far, I thank you for your interest and continued support.
Happy National Diabetes Awareness Month ❤️💙

since 1972

Do you have a story to share about your experiences with diabetes? We want to hear from you! Tell us your story using the form below and we'll consider it for inclusion in the CWD Stories section of our website.